During the current coronavirus pandemic, we wash our hands much more often, and more thoroughly. Effective and frequent hand hygiene is essential to prevent transmission of COVID-19. To get rid of the coronavirus from our hands, we just need water, soap and 30 seconds. In addition to soap, COVID-19 is also deactivated by hand sanitizers containing at least 60% ethanol or 70% isopropanol. This essential preventative practice used to reduce the spread of the virus can also damage the skin. Existing skin conditions, such as atopic dermatitis or psoriasis may also worsen with the use of detergents or disinfectant liquids on the hands. It is important to understand the skin in order to be able to take steps to minimize the impact of frequent handwashing or hand sanitization.
The skin is the largest and one of the most important organs of the human body. It can weigh up to 3 kg and have an area of up to 2m2. It mediates between the body and the external environment and is exposed to many adverse environmental factors every day. The skin protects us against harmful external influences, transmits the most important substances to the appropriate cells and enables the excretion of harmful compounds. To ensure the smooth functioning of the rest of the body, the skin protects us from UV radiation, air pollution, microorganisms (bacteria, viruses or fungi) and other physical, biological or chemical factors. This outermost layer of our body, in cooperation with sweat and sebaceous glands, is also responsible for thermoregulation. It is thanks to our skin, regardless of the temperature of the air that surrounds us, that the temperature of our body is maintained at the same level.
The skin consists of three layers: epidermis, dermis and hypodermis (subcutaneous tissue) and each of them has a different structure and function.
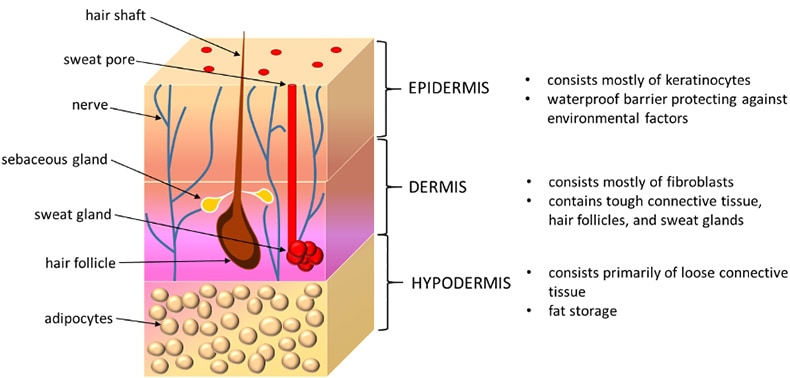
The outermost layer of skin (epidermis) performs a protective function against adverse factors of the external environment. It covers the skin surface tightly and is also the thinnest layer – about 0.5 mm. The epidermis consists of many sublayers and although it may seem like a dead layer, this is not the case.
The epidermis does not have blood vessels, but its deeper levels are very much alive and the layer has self-renewal ability. The main type of cells that form the epidermis (keratinocytes) arise at the very base of the layer, mature, differentiate and gradually migrate towards the surface of the epidermis. The cells become flattened and produce keratin, a substance resistant to chemical agents and insoluble in water. The migration cycle (turnover) is about 28 days.
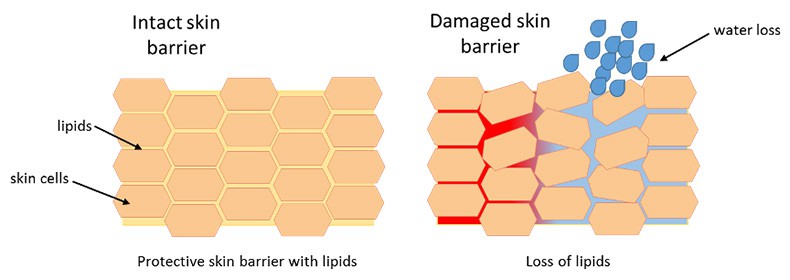
The corneal layer of the epidermis, which is comprised of structural proteins, natural moisturizing factor (NMF) together with a mixture of epidermal lipids, creates the skin protective barrier. Lipids may be produced by skin cells or may come from the lipids delivered to the skin in cosmetics or medicines. The skin lipid barrier is a mixture of many lipids whose proportions and composition change with age or skin condition. The lipid layer consists of ceramides, free fatty acids, cholesterol and its esters, phospholipids, triglycerides and squalene.
Due to the double layer of ceramides, between the cells of the stratum corneum, the skin protective barrier is made impermeable to water and creates a stable, solid structure. It provides protection against adverse external factors. In addition, the lipid coat ensures proper skin hydration by regulating how much water is lost from the skin over time (trans epidermal water loss (TEWL)). A hydrolipid protective layer prevents excessive water loss from the skin.
So, our body has developed a very complex and effective way to ensure that our skin remains hydrated and effective as a barrier. Defects in the functioning or structure of this protective barrier or a decrease in lipid content can contribute to the development of many skin diseases. Most often, the epidermal lipid coat weakens due to adverse external factors, such as the sun (UV radiation), water, low temperatures or wind, to which we are exposed every day. Frequent handwashing with soap or use of strong sanitizers removes the natural lipid layer from the skin, which can cause irritation and even the development of contact dermatitis.
Skin reactions
There are two main types of skin reactions associated with hand hygiene. The most common type includes symptoms such as dryness, irritation, itching, and even cracking and bleeding. This set of symptoms is referred to as irritant contact dermatitis. The second type of skin reaction, allergic contact dermatitis, is less common and is caused by an allergic reaction to some components of hand hygiene products.
Cracked skin increases the risk of local infection. While hand hygiene is essential to prevent the transmission of infections, damaged skin can put people at risk of bacterial infection and some skin viral infections, such as human papillomavirus infection.
There is no ‘skin-friendly’ hand sanitiser because it must contain chemicals to kill the virus but which also dries the skin. They are usually based on ethanol, isopropyl alcohol, chlorhexidine, hydrogen peroxides or quaternary ammonium derivatives. Unfortunately, skin problems associated with strict hand hygiene are inevitable for many people at the moment, especially for health professionals and food industry employees.
Choose the right hygiene product
This is why it is important to choose the right hygiene product. If possible, it is preferable to wash your hands with regular soap instead of using alcohol-based sanitizers. In addition, hands should be moisturized after each wash. Moisturizers are topical products designed to improve and maintain the skin barrier. They work by preventing or reducing water evaporation from the skin – it helps the skin to rehydrate from within.
There are three classes of chemical ingredients that can be used as moisturizers:
- Occlusive (reduce trans-epidermal water loss by forming a hydrophobic barrier film over the skin surface)
- Humectants (hygroscopic substances which attract water and moisture)
- Emollients (cover the skin with a protective film to trap in moisture).
Choosing a cream
A properly selected cosmetic product will be able to restore the natural hydrolipid layer of the epidermis and reduce trans-epidermal water loss. When choosing a cream, it is useful to pay attention to its composition and look for ingredients that will help rebuild the damaged lipid barrier and moisturise the skin. Such substances include lipids (petroleum jelly, glycerin, paraffin, squalane), vitamins (vitamin A, vitamin E), barrier repair ingredients (ceramides, free fatty acids, cholesterol, niacinamide) and moisturizing substances (urea, hyaluronic acid) or soothing ingredients (allantoin, D-panthenol).
Shannon ABC
The choice of the right cleaning agent and the right moisturiser that will restore our skin lipid layer begins in the laboratory. This is where, with the help of modern technology, equipment and knowledge of scientists, we can test if a specific formulation actually benefits the skin lipid layer and restores its protective capabilities. This area is of great interest to Shannon ABC and we have built significant expertise in the area of cosmetic products. Our cosmetics research at Shannon ABC is broadly divided into two parts: cell culture testing for new product development and ingredient screening and skin probe testing for product efficacy validation.
Cell culture testing allows us to test ingredients or final products against skin cells (keratinocytes, fibroblasts) grown in a controlled, sterile laboratory environment. Cell culture testing provides a valuable screening tool with which decisions can be made regarding the performance and impact of an ingredient or product on a skin condition. In laboratory conditions, we can analyze not only the effect of a cosmetic on the epidermal barrier but also keratinocyte or fibroblast proliferation, wound healing properties, anti-inflammatory activity, anti-oxidant protection and anti-wrinkle properties (collagen, elastin production, inhibition of collagenase, elastase). Moreover, we are able to test final products or ingredients on 3-D skin cell models (human skin equivalents), allowing direct application of cosmetic products.
Skin probe testing utilises non-invasive skin testing probes to determine measurements of skin such as skin barrier function, trans-epidermal water loss, elasticity, moisturisation and skin sebum/oil production. Shannon ABC has a reserve panel of approximately 100 volunteers that can be involved in efficacy testing of cosmetic products. Studies range from 24 hours to 4 weeks, depending on requirements, endpoint measures required and products tested.
Hand washing and sanitization are essential treatments to prevent the spread of COVID-19; make sure that you take care of your hands following treatment to ensure that they take care of you!
Find out more about Shannon ABC here. You can also follow them on Twitter for all the latest news.
